Are we sleepwalking into a mental health pandemic just as we see the lights at the end of the COVID-19 Global Pandemic (even if that end is still 6 months away)?
Even before the Pandemic hit the world there was a slow but increasing focus on wellness in the workplace and society in general. But sadly, for many, this was restricted to social media platitudes during mental health week and an 0800 number for employees to call if they felt stressed. For those who “went the extra mile” they may have given their line managers a few hours training on the topic of mental health. A few exemplars introduced further measures for example creating a mechanism for managers and staff to rate/talk about their feelings, often taboo in many workplaces. I do not mean to be overly pessimistic, but we do need to face the reality.
Our wellness really matters and is worth a small fortune!
The World Health Organisation says…
Work is good for mental health, but a negative working environment can lead to physical and mental health problems. (it is also true that a number of variables in our personal lives eg substance abuse, caring responsibilities, relationship difficulties, financial difficulties, etc can also cause mental health problems).
Research shows us that depression and anxiety have a significant economic impact; the estimated cost to the global economy is US$ 1 trillion per year in lost productivity.
And nearly 13% of absence days in the UK are related to mental health issues and specifically stress depression and anxiety. (pre-pandemic)
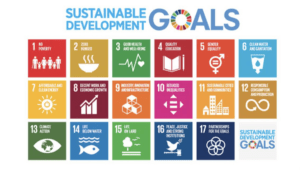
The WHO has created 17 strategic sustainability goals for 2030, and goal number three is: ENSURE HEALTHY LIVES AND PROMOTE WELL-BEING FOR ALL AT ALL AGES.
See below for all the goals.
Working environments have changed over time and this has caused a seismic shift in the psychological contract.” Too many environments in which we work today frustrate our natural inclinations to trust and cooperate.” (Sinek; pg117). This contributes to things like stress, anxiety and depression.
Post the pandemic we have care workers traumatised by all the illness and death they experienced. We have masses of families grieving the loss of a loved one to COVID. And we have a pervasive fear that the virus will spike again as it has done in some countries and some cities. As if that was not enough, we have millions of people around the world facing genuine economic uncertainty as most countries enter economic recession. However bad our wellness was before the pandemic we can be sure that coming out of the crisis it is likely to be far worse for many more.
Our physical and mental health are closely linked at an individual level but we are more practiced at tracking and sharing and talking about our physical health.
Being aware of our own mental health is a lot more difficult. There is no easy tracker. And if we do come to fear that something is wrong, we are less practiced at discussing and sharing it. As individuals, in our families, communities and workplaces we have to change this. If we do not the consequences could be catastrophic. Creating a pervasive environment where it is OK not to be OK is vital I think for the next phase most countries are entering.
With advancements in personal physical heath I can monitor and share me steps, heart rate, calories, sleep, etc daily, (see left – I must have had a busy week), and with a new inexpensive device, take my own clinically sound ECG whenever I want to. See example to below. But monitoring our mental health and well being is much more complex.
Being able to easily track and share all this information is fast becoming the norm and is no doubt assisting people in getting and keeping healthy. With the obesity crisis this is essential. But this is not at all what its like for mental health. Difficult to assess and measure, and very difficult to share and talk about.
Sinek says; “Leadership is not being in charge, it is about taking care of people in your charge”.
But the Pandemic has essentially put the global economy into recession and the uncertainty will likely in the short term at least be replaced for many by redundancy or under-employment. “Many studies demonstrate that being laid off increases a person’s risk of dying compared with people who are not laid off”(Pfeffer; pg74) and goes on to say that data shows very clearly that being laid off from your job significantly increases the risk of suicide together with depression, anxiety and a host of other ailments.
I am not sure we are prepared for this even though this deterioration in mental well being is completely predictable and for the most part an acceleration of an existing trend.
So, what might we consider, here are some ideas but we need a comprehensive holistic approach:
- Make sure levels of psychological safety are such that people feel that they can be open about all issues, including mental health at least in the workplace. Do the same in our personal lives with family, friends, clubs and societies etc. It should be part of the curriculum in schools and universities.
- Focus on mental health issues 24/7/365 – because that is how sufferers experience their disability. Not just for one week a year when social media gives you exposure. Do so from a wellness perspective which focuses on being better.
- Educate line managers and HR professionals and (health care professions and teachers, and ministers, husbands, wives etc) on how to deal productively with people suffering from a mental illness. This starts with identification and then learning how to have proper meaningful conversations.
- That includes developing mechanisms for early detection and some way of measuring the wellness of your workforce on an ongoing basis.
- Track and manage your data properly, but treat people who disclose they are suffering from mental health issues as individuals.
- Make sure your outsource provider of health/mental health services is properly equipped to deal with your employees who need help and ensure a close relationship between your provider and your organisation (including data and trend analysis and awareness training).
- Act now – it is already almost too late!
Andrew Fox, www.rhinohr.co.uk
References:1. https://www.mentalhealth.org.uk/statistics/mental-health-statistics-mental-health-work2. https://www.who.int/mental_health/in_the_workplace/en/3. Sinek, Simon; Leaders Eat Last;(2014); Penguin, USA4. Pfeffer, Jeffrey, Dying for a Paycheck, (2018) Harper Collins, USA, NY
This article is exclusive to The Business Transformation Network.